Ashley St. Pierre, a Team IMPACT masters-level social work intern, has lived with cystic fibrosis (CF) since she was just three months old. CF is a progressive, genetic disease that affects the lungs and other organs and leads to a variety of complications. CF can be isolating, but like many of the children in our program, Ashley has found her communities and support systems in unexpected places.
For Ashley, those places span the east coast. She enjoys moving and has lived in many different states, including Georgia, Florida, Connecticut, New York, North Carolina, and Massachusetts. When she was a kid, she found community in her horse barn. She rode a horse for the first time when she was five years old and only took a break when she decided she wanted to have a “normal social life.”
She found community in school. She has a bachelor’s degree in English and master’s degrees in journalism and school counseling. It was actually because of CF that Ashley left the school environment—she was following her doctors’ advice to avoid germy environments because of her immunocompromised state—and decided to go back to school for yet another master’s degree—this time in social work.
Ashley found community through her medical journey. She received a double lung transplant in May of 2018 and credits the incredible care of her medical team, counselor, and social worker with inspiring her to become a social worker herself.
Ashley’s life path led her up and down the east coast, in and out of school, in and out of hospitals, and eventually, to Team IMPACT. In her work as a master’s level social work intern at Team IMPACT, she works closely with other members of our clinical team. In recognition of Cystic Fibrosis Awareness Month this May, we sat down with Ashley to talk about her lifelong journey with cystic fibrosis and how the disease shaped her into who she is today.



When I found out about an internship opportunity at Team IMPACT, I was very excited because I love kids and I love working with chronically ill populations. I directly experienced how inspiring working with an athletic team can be, as I was a poster child for the Atlanta Braves for a few years during my childhood. I just remember really amazing memories from that time period, and it was an experience that I cherish. With my background and life experiences, Team IMPACT just seemed like a perfect fit. I am very passionate about counseling, and eventually my goal is to work with a population that is chronically ill.
I was diagnosed with cystic fibrosis at three months old. Growing up with CF required taking a lot of daily pills, including enzymes every time you eat and insulin if you also have CF-related diabetes (CFRD). It also meant I had to do breathing treatments two to four times a day, got admitted to the hospital for IV antibiotics for roughly two to three weeks at a time a few times a year, underwent regular sinus surgeries, and eventually, also received a double lung transplant on May 15, 2018.



I needed the transplant due to the natural course of CF’s progression in my lungs. The experience was slightly surreal. When I got the call, I had only been listed on the transplant list for a week, so I thought it would just be a dry run. Typically, you are informed that this scenario might happen a few times before you actually get lungs that they can transplant. Oftentimes for CF patients awaiting a lung transplant, you are called to come to the hospital because the medical team thinks they have a potential set of lungs that are a match. You will start prepping for the surgery, but then, after examining the lungs, the surgeon decides that they do not want to move forward, for some reason or another. The “prepping for surgery” process involves drinking a huge jug of fluid right when you get to the hospital, which in itself is a challenge. I feel like I was really just focusing on drinking that liquid, thinking that this was good practice for when I would have to come back and do it for real.
Then my family members started showing up, and I was told the lungs were good to go and that the surgery would be happening that day. Thankfully, I was thinking too much about my family to really think about the surgery at the time, and then I was put under before I could really get nervous about it, which I now think was a blessing.
After I woke up from surgery, I felt amazing. I was up and walking shortly thereafter, which is what my medical team was striving for. The first two weeks went well. They were about to release me, but then I started having complications. I needed more chest tubes put in, I had to do multiple spinal taps, I had a blood clot in my chest that needed to clear, the list goes on. I ended up staying in the hospital for six or seven weeks post-transplant. Eventually, I started wondering if I would ever leave. But I did.


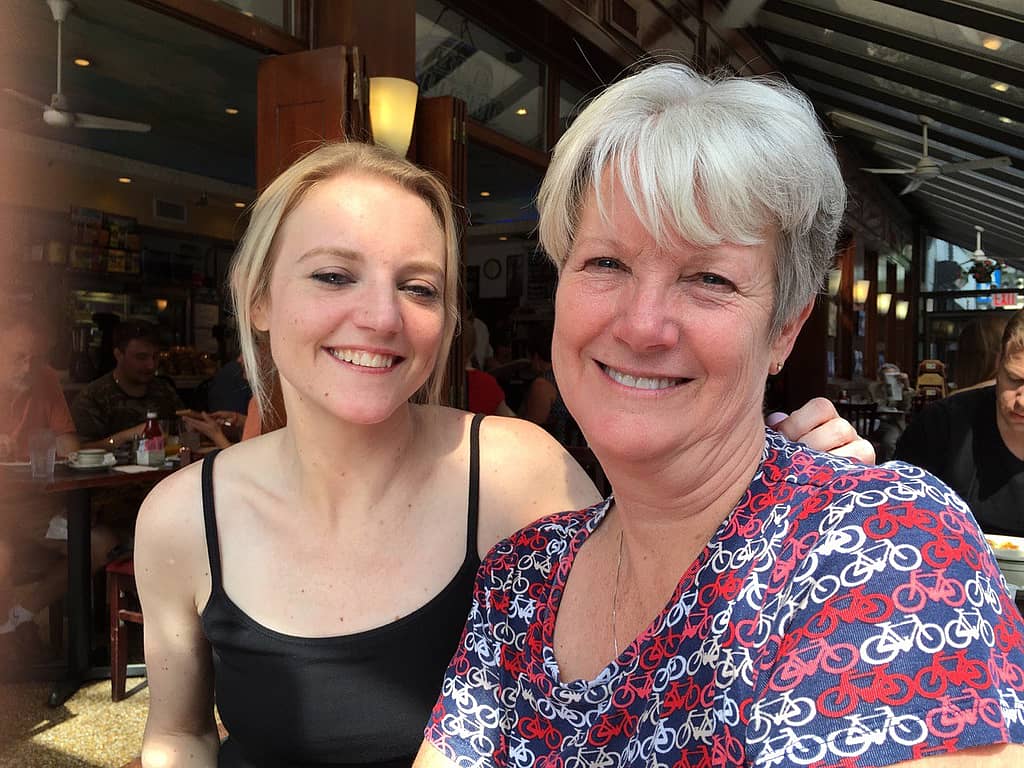
The recovery was a bit slow for me. I spent a year living with my mother (it is required to live with a primary caregiver for a year after transplant) in an apartment close to the hospital, doing physical therapy and all the necessary protocols. It was difficult to establish the right doses for the anti-rejection medications, which are still monitored with monthly labs, but we were able to get to the right dose eventually. I had one experience of rejection, which was suppressed by high-dose IV steroids, and many other random setbacks; but after a year, I was feeling pretty good.
Before the surgery, I was in a bit of denial regarding the fact that I needed a transplant. I knew it was something that would likely happen down the road, but I felt way too healthy at the time. Looking back, I realize I was actually not healthy at all but was just so used to feeling the way I did that thought I was fine. I was living in New York City at the time and had gotten used to dragging oxygen bottles around with me. I moved down to North Carolina to do the transplant at UNC because my family was nearby and I trusted the medical team there. There is a very fine window when it comes to transplants—you do not want to do it prematurely, but you do want to do it while you’re strong and healthy enough to heal from it. Luckily, we hit that window with my transplant.
Today, nearly five years later, I am feeling good. I notice that I do not have the same degree of energy that I had before, but it is amazing to not have to do treatments or constantly cough. I remember my coughing fits were so bad that I would get off the subway at a random stop because I did not want to scare anyone on the train with me. Some people say that transplant is like trading one disease in for another, and I agree with that. It is like gaining an entirely new set of medical issues, but for me, it was necessary for survival. Getting a transplant is a very individualized experience; some have no issues with it and have adjusted beautifully afterwards, and then some do not survive. Getting a double lung transplant is not to be taken lightly and is not without risk. Although the experience is extremely challenging and life-changing, I would do it again in a heartbeat.


If I could give my younger self advice about this experience, I would say to just take care of yourself. Take all your pills, do all the treatments, and avoid being around second-hand smoke. Most of all, I would advise not living your life in a bubble but living your life to the fullest. Travel as much as possible if that interests you. Follow your passions and desires. Plan like you will live forever, but live like you could die tomorrow, because any of us—living with a disease like cystic fibrosis or not—could.
It can be challenging to have an “invisible illness,” especially if you do not know what to look for. You cough a lot when you have CF, but that does not mean you are sick or that you will make others sick. It’s hard to explain to strangers and also hard for them to understand. Sometimes people may think that I am lazy, unmotivated, or just like to complain rather than understanding that I might just be exhausted because of what my body is fighting on the inside or that I am experiencing significant pain. I do not think that the average person understands everything that goes into fighting this disease, especially in terms of the time and resources that are involved.
It can be so beneficial to connect with others that are going through a similar experience. The CF community is amazing and extremely supportive. Within the CF community are a lot of groups that can help provide knowledge, resources, and other people sharing their journey of living with CF. Team IMPACT and like-minded organizations are so pivotal to members of the CF community because they help support and foster individual social and emotional growth in kids that are living with chronic illness. Participating in Team IMPACT means gaining a new social support network and sense of belonging, giving kids something positive to look forward to, and focus on other than doctor appointments and hospitalizations.



